Abstract
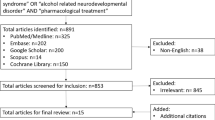
Fetal Alcohol Spectrum Disorders affect up to 5% of the population, with additional children affected by prenatal drug exposures. The majority of these children display symptoms of ADHD and poor emotional dysregulation, a common reason for seeking psychiatric care. However, high prevalence of comorbid look-alike symptoms and limited availability of evidence-based treatments complicates psychiatric decision making in this population. The goal of the current study is to report on the effectiveness of psychotropic medications in a case series of 16 individuals with prenatal alcohol/drug exposure and propose a model for psychiatric care for this population. In addition to traditional subjective reports, an objective continuous performance test (T.O.V.A.®) was used to aid with guiding treatment. We found that T.O.V.A.®-scores improved on average from − 6.5 to − 2.9 with our psychiatric approach (p = 0.03). T.O.V.A.®-measurements were helpful in differentiating ADHD symptoms from comorbid symptoms and to guide decision-making on starting and changing medications.


Similar content being viewed by others
References
May PA, Chambers CD, Kalberg WO, Zellner J, Feldman H, Buckley D et al (2018) Prevalence of Fetal Alcohol Spectrum Disorders in 4 US Communities. JAMA 319:474–482
Makadia LD, Roper PJ, Andrews JO, Tingen MS (2017) Tobacco use and smoke exposure in children: new trends, harm, and strategies to improve health outcomes. Curr Allergy Asthma Rep 17:55
Buckingham-Howes S, Berger SS, Scaletti LA, Black MM (2013) Systematic review of prenatal cocaine exposure and adolescent development. Pediatrics 131:e1917-1936
O’Connor MJ, Paley B (2009) Psychiatric conditions associated with prenatal alcohol exposure. Dev Disabil Res Rev 15:225–234
Mattson SN, Bernes GA, Doyle LR (2019) Fetal Alcohol Spectrum Disorders: a review of the neurobehavioral deficits associated with prenatal alcohol exposure. Alcohol Clin Exp Res 43:1046–1062
Jones KL (2011) The effects of alcohol on fetal development. Birth Defects Res C Embryo Today 93:3–11
Mukherjee RAS, Cook PA, Norgate SH, Price AD (2019) Neurodevelopmental outcomes in individuals with Fetal Alcohol Spectrum Disorder (FASD) with and without exposure to neglect: clinical cohort data from a national FASD diagnostic clinic. Alcohol 76:23–28
Chambers CD, Coles C, Kable J, Akshoomoff N, Xu R, Zellner JA et al (2019) Fetal Alcohol Spectrum Disorders in a Pacific Southwest City: maternal and child characteristics. Alcohol Clin Exp Res 43:2578–2590
Fryer SL, McGee CL, Matt GE, Riley EP, Mattson SN (2007) Evaluation of psychopathological conditions in children with heavy prenatal alcohol exposure. Pediatrics 119:e733-741
Frankel F, Paley B, Marquardt R, O’Connor M (2006) Stimulants, neuroleptics, and children’s friendship training for children with Fetal Alcohol Spectrum Disorders. J Child Adolesc Psychopharmacol 16:777–789
Ritfeld GJ, Kable JA, Holton JE, Coles CD (2022) Psychopharmacological treatments in children with Fetal Alcohol Spectrum Disorders: a review. Child Psychiatry Hum Dev 53:268–277
Oesterheld JR, Kofoed L, Tervo R, Fogas B, Wilson A, Fiechtner H (1998) Effectiveness of methylphenidate in Native American children with fetal alcohol syndrome and attention deficit/hyperactivity disorder: a controlled pilot study. J Child Adolesc Psychopharmacol 8:39–48
O’Malley KD, Koplin B, Dohner VA (2000) Psychostimulant clinical response in fetal alcohol syndrome. Can J Psychiatry 45:90–91
Doig J, McLennan JD, Gibbard WB (2008) Medication effects on symptoms of attention-deficit/hyperactivity disorder in children with Fetal Alcohol Spectrum Disorder. J Child Adolesc Psychopharmacol 18:365–371
Snyder JNJ, Snyder R, Block G (1997) A study of stimulant medication in children with FAS. In: Streissguth AKJ (ed) Overcoming and preventing secondary disabilities in fetal alcohol syndrome and fetal alcohol effects. University of Washington Press, Seattle, pp 64–77
Coe JSJ, Riley K, Waltermire J, Hagerman R (2001) A survey of medication responses in children and adolescents with fetal alcohol syndrome. Mental Health Aspects Dev Disabil 4:148–155
Pliszka S (2007) Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 46:894–921
Coles CD, Platzman KA, Raskind-Hood CL, Brown RT, Falek A, Smith IE (1997) A comparison of children affected by prenatal alcohol exposure and attention deficit, hyperactivity disorder. Alcohol Clin Exp Res 21:150–161
Wozniak JR, Fuglestad AJ, Eckerle JK, Fink BA, Hoecker HL, Boys CJ et al (2015) Choline supplementation in children with Fetal Alcohol Spectrum Disorders: a randomized, double-blind, placebo-controlled trial. Am J Clin Nutr 102:1113–1125
Nguyen TT, Risbud RD, Mattson SN, Chambers CD, Thomas JD (2016) Randomized, double-blind, placebo-controlled clinical trial of choline supplementation in school-aged children with Fetal Alcohol Spectrum Disorders. Am J Clin Nutr 104:1683–1692
Wozniak JR, Fink BA, Fuglestad AJ, Eckerle JK, Boys CJ, Sandness KE et al (2020) Four-year follow-up of a randomized controlled trial of choline for neurodevelopment in Fetal Alcohol Spectrum Disorder. J Neurodev Disord 12:9
Mela M, Okpalauwaekwe U, Anderson T, Eng J, Nomani S, Ahmed A et al (2018) The utility of psychotropic drugs on patients with Fetal Alcohol Spectrum Disorder (FASD): a systematic review. Psychiatry Clin Psychopharmacol 28:436–445
Elliott CD (2007) Differential ability scales (2nd ed). Can J School Psychol 22:128–132.
Sparrow S, Balla D, Cichetti, D (1984) The vineland adaptive behavior scales: american guidance service. Circle Pines
Fernhoff PM, Smith IE, Falek A (1980) Dysmorphia checklist. Document available through the maternal substance abuse and child development project. Division of Psychiatry, Emory University, Atlanta
Coles CD, Gailey AR, Mulle JG, Kable JA, Lynch ME, Jones KL (2016) A comparison among 5 methods for the clinical diagnosis of Fetal Alcohol Spectrum Disorders. Alcohol Clin Exp Res 40:1000–1009
Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB et al (2001) Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry 40:168–179
Coles CD, Kable JA, Taddeo E, Strickland DC (2015) A metacognitive strategy for reducing disruptive behavior in children with Fetal Alcohol Spectrum Disorders: GoFAR pilot. Alcohol Clin Exp Res 39:2224–2233
Achenbach TM (2017) Achenbach system of empirically based assessment (ASEBA). In: Kreutzer J, DeLuca J, Caplan B (eds) Encyclopedia of clinical neuropsychology. Springer, Cham, pp 1–7
Greenberg LM (2011) The test of variables of attention (version 8.0) [computer software]. The TOVA Company, Los Alamitos
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B (Methodol) 57:289–300
Randall S, Hannigan JH (1999) In utero alcohol and postnatal methylphenidate: locomotion and dopamine receptors. Neurotoxicol Teratol 21:587–593
Hannigan JH, Pilati ML (1991) The effects of chronic postweaning amphetamine on rats exposed to alcohol in utero: weight gain and behavior. Neurotoxicol Teratol 13:649–656
Ulug S, Riley EP (1983) The effect of methylphenidate on overactivity in rats prenatally exposed to alcohol. Neurobehav Toxicol Teratol 5:35–39
Means LCM, Hughes V, Grey K (1984) Rats exposed in utero to ethanol are hyperresponsive to methylphenidate when tested as neonates or adults. Neurobehav Toxicol Teratol 6:187–192
Juarez J, Guerrero-Alvarez A (2015) Effects of methylphenidate and atomoxetine on impulsivity and motor activity in preadolescent rats prenatally-treated with alcohol. Behav Neurosci 129:756–764
Glass L, Graham DM, Deweese BN, Jones KL, Riley EP, Mattson SN (2014) Correspondence of parent report and laboratory measures of inattention and hyperactivity in children with heavy prenatal alcohol exposure. Neurotoxicol Teratol 42:43–50
Hanlon-Dearman A, Chen ML, Olson HC (2018) Understanding and managing sleep disruption in children with Fetal Alcohol Spectrum Disorder. Biochem Cell Biol 96:267–274
Durr MR, Petryk S, Mela M, Des Roches A, Wekerle M, Newaz S (2021) Utilization of psychotropic medications in children with FASD: a retrospective review. BMC Pediatr 21:512
Funding
Funding for this study was provided by a grant from the Department of Behavioral Health and Developmental Disabilities, State of Georgia, Contract # 44100-907-0000056259, NIH/NIAAA Diversity Supplement 3U01AA026108-04S1A and the American Academy of Child and Adolescent Psychiatry (AACAP) Pilot Research Award for Junior Faculty and Child and Adolescent Psychiatry Fellows, supported by AACAP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All Authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ritfeld, G.J., Kable, J.A., Holton, J.E. et al. Effectiveness of Psychotropic Medications in Children with Prenatal Alcohol and Drug Exposures: A Case Series and Model of Care. Child Psychiatry Hum Dev (2022). https://doi.org/10.1007/s10578-022-01451-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s10578-022-01451-3